Abstract
Background: Adult T-cell leukemia/lymphoma (ATLL) is a rare mature T-cell malignancy driven by the human T-cell lymphotropic virus type I (HTLV-1) that remains challenging to treat and is associated with a dismal prognosis. While some reports have shown encouraging results with allogeneic stem-cell transplantation (allo-SCT), data remains scarce and mostly limited to Japanese patients.
Patients and Methods: This is a retrospective single center analysis with 100 HTLV-1-associated North American ATLL patients. Variables collected included age, sex, ethnicity, CMV/HTLV1 serologies, karnofsky performance score (KPS), diagnosis date, disease subtype, number of prior therapy lines, transplant type, status at transplant, transplant date, prior SCT, donor sex, CMV/HTLV1 serologies, stem cell source, donor type, in-vivo T-cell depletion, engraftment, conditioning regimen, GVHD prophylaxis, maximum acute and chronic GVHD grade, relapse date when applicable, and main cause of death. The Kaplan-Meier method was used to calculate overall survival (OS) and progression-free survival (PFS). Cumulative incidence functions were used to estimate relapse incidence (RI) and non-relapse mortality (NRM) in a competing risk setting. Death and relapse were considered as competing events for acute and chronic GVHD. Univariate analyses were done using the Gray's test for cumulative incidence functions and the log rank test for OS and PFS. A Cox proportional hazards model was used for multivariate regression, results were expressed as hazard ratio (HR) with a 95% confidence interval (CI). All tests were two-sided, type-1 error was fixed at 5%.
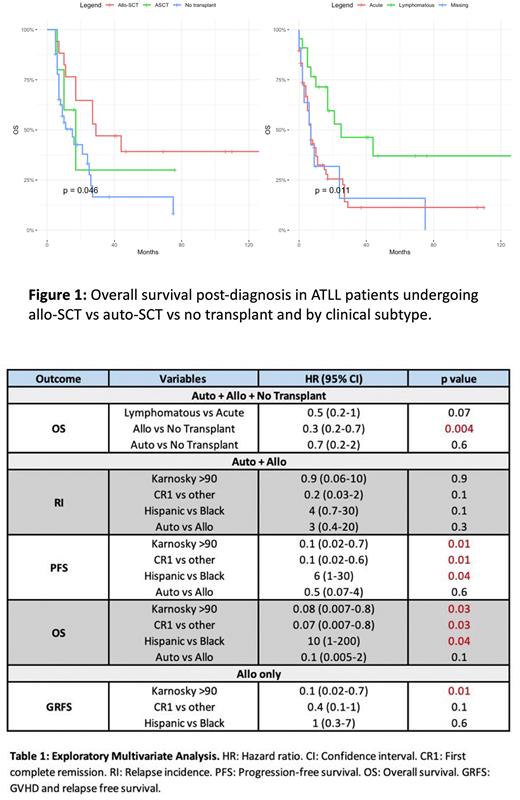
Results: One hundred patients met eligibility criteria, 18-87 years old, 69 of which were Black, 27 Hispanic, and 2 of Asian descent. Sixty-seven patients had acute ATLL and 22 lymphomatous. In total, 22 patients underwent SCT with 17 allo-SCT and 5 autologous SCT (ASCT) between 2005-2020 with a median follow-up of 62 months. Ten patients (45%) were transplanted in first complete remission (CR1), and 15 (68%) had KPS ≥90. Among patients undergoing allo-SCT, 41% had matched sibling donors (MSD), 18% matched unrelated (MUD), and 35% haploidentical. The 1-year and 3-years rates of overall survival from diagnosis of the cohort were 42% and 21%, respectively. Acute ATLL subtype was a strong predictor of worse outcome (Figure 1) with 1-year and 3-years OS of 32% vs 71% (p=0.004) and 11% vs 46% (p=0.002), respectively, compared to lymphomatous disease. To account for immortal time bias, 37 non-transplanted patients with early mortality within 4 months of diagnosis that were not able to make it to transplant were excluded from the Kaplan-Meier survival analysis. Patients undergoing transplant had improved outcomes compared to non-transplanted patients (Figure 1, Table 1), with allo-SCT reaching statistical significance in multivariate analysis compared to the non-transplant group with OS HR of 0.3 (p=0.004) compared to 0.7 (p=0.6) in ASCT vs non-transplant. In transplanted patients, the 3-year RI and NRM were 51% and 37%, respectively, and 3-year PFS and OS were 31% and 39%, respectively. Four of five patients who received ASCT rapidly relapsed with 3 dying from disease progression and one lost to follow-up, with 1-year RI of 80% vs 30% in allo-SCT (p=0.03). In exploratory multivariate analysis, patients achieving CR1 and with good baseline performance scores (KPS >90) had significantly better outcomes compared to their counterparts regardless of transplant type, and surprisingly, race was a strong and significant predictor of outcomes affecting PFS and OS with Hispanic vs Black PFS and OS HRs of 6 (p=0.04) and 10 (p=0.04), respectively. Thirteen patients died within 2 years, eight from relapse/progression including 3 ASCT patients, and 4 from transplant-related toxicities.
Conclusion: Our data suggest that allo-SCT, but not ASCT, is a valid option in select ATLL patients. It also appears that patients of Hispanic descent have worse outcome post-transplant but not overall, which could be explained by lack of compatible donors or barriers to early transplant. Although this is the largest NA-ATLL transplant cohort presented to date outside of Japan and Europe, further studies are necessary to fully explain these discrepancies.
Disclosures
Bazarbachi:ASH: Research Funding. Shah:MashUpMD: Honoraria; Bristol Myers Squibb: Consultancy, Research Funding; MJH Lifesciences: Consultancy, Honoraria; ACCC: Honoraria; Janssen: Consultancy, Research Funding; Sanofi: Consultancy. Shastri:Janssen: Consultancy; Rigel Pharmaceutical: Membership on an entity's Board of Directors or advisory committees; NACE: Honoraria; Kymera Therapeutics: Membership on an entity's Board of Directors or advisory committees, Research Funding. Verma:Throws Exception: Current equity holder in publicly-traded company; Stelexis Therapeutics: Consultancy; Stelexis Therapeutics: Current equity holder in publicly-traded company; Eli Lilly and Company: Research Funding; Jannsen: Research Funding; Incyte: Research Funding; Acceleron Pharma: Consultancy; MedPacto: Research Funding; Celgene: Consultancy, Research Funding; Novartis: Consultancy, Research Funding; GlaxoSmithKline: Research Funding; BMS: Research Funding; Curis: Research Funding. Janakiram:Janssen: Consultancy, Membership on an entity's Board of Directors or advisory committees, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal